Antral Follicle Count (AFC) is a transvaginal ultrasound measurement that counts small ovarian follicles early in the menstrual cycle to estimate ovarian reserve. It helps predict response to fertility treatments such as IVF, guides reproductive planning, and identifies possible hormonal conditions affecting the ovaries.
Typical reproductive-age counts often fall between 10 and 20 follicles total, counts under roughly 6–10 may indicate reduced ovarian reserve, and counts above 20 follicles can reflect strong reserve or endocrine conditions such as polycystic ovarian syndrome.
AFC is useful clinically but it cannot reliably predict natural pregnancy chances, egg quality, or exact fertility timeline because reproductive success depends on multiple biological factors beyond follicle quantity.
What the AFC Actually Measures
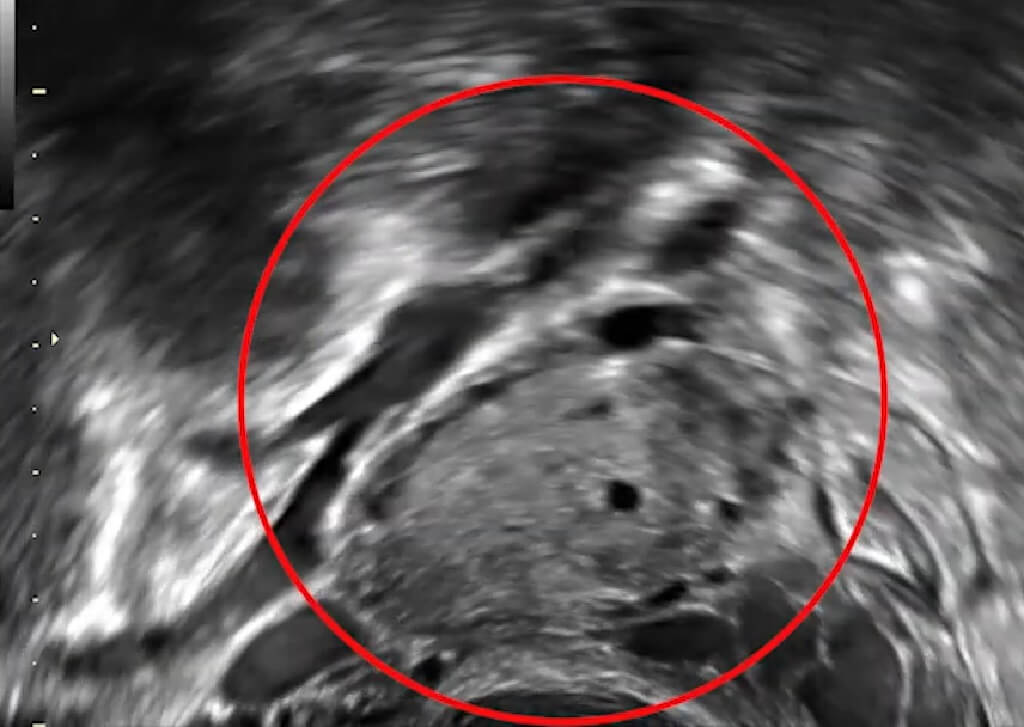
Antral follicles are small fluid-filled structures in the ovaries that each contain an immature egg. They are visible through ultrasound when they reach approximately 2–10 millimeters in diameter. The number of these follicles correlates with the remaining pool of primordial follicles, which gradually declines with age. AFC therefore acts as a proxy for ovarian reserve rather than a direct measure of fertility.
Clinically, AFC is measured during the early follicular phase of the menstrual cycle, typically days 2 through 5, when hormonal activity is relatively stable. Measuring outside this window may produce misleading counts because dominant follicles or luteal activity can obscure smaller follicles.
From a physiological standpoint, only a fraction of follicles ever mature to ovulation. Most undergo natural degeneration through a process called atresia. AFC therefore reflects potential ovarian responsiveness rather than the number of eggs that will actually ovulate or fertilize.
The test is widely used because it is non-invasive, relatively inexpensive compared with laboratory fertility testing, and provides immediate visual confirmation of ovarian structure and follicle distribution.
Typical AFC Number Ranges and Clinical Meaning

Interpretation of AFC values varies slightly among fertility clinics, but broad clinical ranges are well established. These ranges reflect ovarian reserve trends observed across population studies.
AFC Interpretation Table
| AFC Total Count | Interpretation | Clinical Implication |
| 0–4 | Very low ovarian reserve | Reduced response expected in IVF |
| 5–9 | Low reserve | Possible fertility challenges |
| 10–20 | Normal reserve | Typical reproductive range |
| 21–30 | High reserve | Strong treatment response likely |
| >30 | Very high reserve | Possible PCOS or hyperstimulation risk |
Counts below approximately six follicles often correlate with diminished ovarian reserve and may signal a lower response to ovarian stimulation medications. Conversely, high counts do not necessarily mean higher fertility. Elevated AFC may reflect hormonal imbalance, irregular ovulation, or metabolic conditions.
Clinical interpretation always includes patient age, hormone levels such as AMH (Anti-Müllerian Hormone), and reproductive history.
Age-Related AFC Trends
Age remains the strongest predictor of ovarian reserve. AFC typically declines gradually beginning in the late twenties, with acceleration after age 35.
Average AFC by Age
| Age Range | Typical AFC Average |
| 20–24 | 16–25 follicles |
| 25–34 | 13–20 follicles |
| 35–39 | 10–15 follicles |
| 40–44 | 6–10 follicles |
| 45+ | 3–6 follicles |
The decline reflects the natural depletion of the ovarian follicle pool. Individuals are born with roughly one to two million primordial follicles, decreasing to about 300,000 by puberty. Only about 300–400 ovulate during reproductive life, while the rest undergo gradual atresia.
Importantly, variability is substantial. Some individuals maintain relatively high counts into their late thirties, while others experience earlier decline due to genetics, autoimmune conditions, surgery, or environmental exposures.
AFC and Fertility Treatment Planning

AFC plays a major role in assisted reproductive technology because it predicts ovarian response to stimulation medications used during IVF cycles. Patients with low counts may require higher medication doses and may produce fewer eggs, while high counts increase the risk of ovarian hyperstimulation syndrome.
Typical clinical use includes:
- Determining medication dosage for ovarian stimulation
- Predicting egg retrieval yield
- Estimating IVF success probabilities
- Identifying endocrine disorders affecting fertility
In cases of significantly diminished ovarian reserve where egg production becomes unreliable, reproductive specialists sometimes discuss alternatives such as IVF with donor oocytes, particularly when age-related egg quality decline or ovarian depletion reduces chances of success using autologous eggs. This option shifts focus from egg quantity toward embryo viability while maintaining pregnancy potential through uterine health.
This demonstrates how AFC informs treatment direction rather than defining reproductive outcomes alone.
Relationship Between AFC and Egg Quality
A critical distinction often misunderstood is that AFC reflects egg quantity, not egg quality. Egg quality declines primarily with age due to increased chromosomal abnormalities, mitochondrial dysfunction, and cumulative environmental exposure.
A person with a high AFC in their forties may still face reduced fertility because egg quality diminishes independently of follicle number. Conversely, a younger individual with a low AFC may still achieve pregnancy due to better egg quality.
This explains why AFC alone cannot predict miscarriage risk, embryo viability, or genetic health of eggs.
AFC Compared With Other Ovarian Reserve Tests
Clinicians usually combine AFC with hormonal testing for more accurate assessment.
Ovarian Reserve Test Comparison
| Test | Measurement Type | Key Advantage | Limitation |
| AFC Ultrasound | Follicle visualization | Direct ovarian imaging | Operator dependent |
| AMH Blood Test | Hormone from follicles | Stable across cycle | Lab variability |
| FSH Blood Test | Pituitary response | Long clinical history | Cycle dependent |
| Estradiol Level | Hormonal activity | Useful adjunct marker | Less predictive alone |
Combining AFC and AMH is often considered the most reliable method for estimating ovarian reserve because both reflect follicular pool size through different mechanisms.
What the AFC Cannot Predict
Despite widespread clinical use, AFC has limitations that must be understood to avoid misinterpretation.
Limitations Table
| Fertility Factor | AFC Predictive Value |
| Natural pregnancy likelihood | Limited |
| Egg genetic health | None |
| Implantation success | Indirect |
| Male fertility contribution | None |
| Exact menopause timing | Approximate only |
Natural conception depends on ovulation quality, sperm parameters, uterine environment, hormonal balance, and timing of intercourse. AFC contributes only one piece of this complex system.
Menopause timing is influenced by long-term follicle depletion patterns that AFC snapshots cannot fully capture.
Conditions That Affect AFC Results
Certain medical conditions can distort follicle counts or their interpretation.
Polycystic ovarian syndrome often produces elevated AFC due to the accumulation of small follicles that fail to mature. Endometriosis, prior ovarian surgery, chemotherapy, or autoimmune disease can reduce counts prematurely.
Lifestyle factors such as smoking, obesity, chronic stress, and environmental toxin exposure have also been associated with reduced ovarian reserve in epidemiological studies.
These influences highlight why AFC interpretation must consider the full medical context rather than isolated numbers.
Clinical Accuracy and Variability
AFC reliability depends partly on ultrasound technique and practitioner experience. Differences in equipment resolution, probe angle, and follicle measurement criteria can cause variability between clinics.
Cycle-to-cycle variation also occurs. A single AFC measurement may differ slightly month to month due to transient hormonal changes. Repeated testing sometimes provides a more stable assessment when clinical decisions depend heavily on ovarian reserve estimation.
Standardized measurement protocols improve consistency, but absolute precision remains limited.
Psychological Impact of AFC Results

Fertility testing often carries emotional weight. Numeric AFC results can trigger anxiety because they appear definitive. However, reproductive biology involves probabilities rather than certainties.
Low AFC does not eliminate the possibility of pregnancy. Many individuals conceive naturally despite reduced ovarian reserve, particularly at younger ages. Similarly, high AFC does not guarantee success if other fertility factors are present.
Accurate counseling emphasizes that AFC guides decisions but does not determine reproductive destiny.
Research Insights and Statistical Context
Population research consistently confirms a correlation between AFC and ovarian reserve decline with age. Studies suggest average AFC decreases roughly one follicle per year after early adulthood, although the slope varies by individual.
Clinical IVF data show:
- Higher AFC correlates with greater egg retrieval numbers
- Optimal IVF outcomes often occur with moderate counts rather than extremes
- Extremely high counts increase hyperstimulation risk
- Extremely low counts reduce medication responsiveness
However, pregnancy rates depend more heavily on embryo quality and uterine receptivity than follicle number alone.
Practical Takeaways for Patients
Understanding AFC results involves interpreting them as one data point within a broader reproductive assessment.
Key clinical interpretations include:
- Normal counts suggest a typical ovarian reserve for age
- Low counts prompt evaluation of the fertility timeline
- High counts may require hormonal evaluation
- Trends over time matter more than single measurements
Early fertility consultation can help contextualize results and explore options if reserve decline is suspected.
Final Clinical Perspective
Antral Follicle Count remains one of the most informative non-invasive indicators of ovarian reserve available in reproductive medicine. It provides immediate visual assessment of follicle quantity, supports fertility treatment planning, and offers insight into reproductive aging patterns.
Typical counts cluster around 10–20 follicles in reproductive-age individuals, lower numbers often indicate diminished reserve, and elevated counts may reflect strong reserve or endocrine conditions.
However, AFC cannot determine egg quality, predict natural conception reliably, or define reproductive lifespan with precision. Fertility outcomes depend on multiple interacting biological factors, including age, genetics, hormonal balance, sperm health, uterine environment, and overall health status. AFC is best understood as a clinical guidance tool rather than a definitive fertility predictor.















