The gallbladder is a small, pear-shaped organ situated beneath the liver. Its primary function is to store and concentrate bile, a fluid produced by the liver that aids in the digestion of fats.
A contracted gallbladder, often detected during medical imaging tests, is a condition where the gallbladder appears shrunken or smaller than usual. This condition can be a normal response to physiological factors, such as having eaten a meal, or it could indicate certain health issues.
Causes of Gallbladder Contraction

A contracted gallbladder can result from various causes. In many cases, it’s simply a response to a meal. After eating, the gallbladder contracts to release bile into the small intestine to assist in digestion. However, in some instances, a persistently contracted gallbladder could indicate gallbladder disease or other issues.
Chronic gallbladder disease, gallstones, or inflammation (cholecystitis) can lead to abnormal contraction. Additionally, other conditions such as biliary dyskinesia, where the gallbladder does not empty properly, may also be responsible, according to PubMed.
Symptoms and Signs

A contracted gallbladder is frequently asymptomatic, particularly when it occurs as a normal physiological response after eating. In healthy individuals, the gallbladder contracts to release bile into the digestive tract, aiding in the breakdown of dietary fats—this usually happens without any discomfort or noticeable symptoms. According to the Mayo Clinic and Johns Hopkins Medicine, this postprandial contraction is a regular part of digestion.
However, when the gallbladder contracts due to an underlying issue, symptoms can become apparent. For example, when gallstones or inflammation (cholecystitis) are present, contraction can trigger classic signs of gallbladder disease. Studies published in the NCBI report the following common symptoms:
-
Pain in the upper right or middle abdomen: Often described as sharp, cramping, or squeezing. This pain may be episodic (biliary colic) or persistent, especially if there is an obstruction, and it can radiate to the right shoulder or back.
-
Nausea and vomiting: These symptoms frequently accompany gallbladder pain, particularly after meals rich in fat. In a study by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), over 70% of patients with symptomatic gallbladder disease reported post-meal nausea.
-
Discomfort after fatty foods: According to the Cleveland Clinic, meals high in fat can prompt intense gallbladder contractions, aggravating pain and discomfort in those with underlying disease.
According to a 2023 analysis in BMJ, up to 15% of adults will develop gallstones, yet most remain asymptomatic until stones obstruct the bile duct or inflammation develops.
Diagnostic Procedures
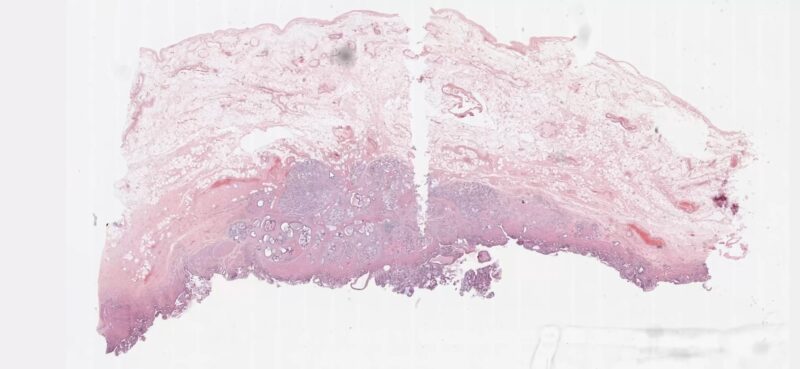
The diagnosis of a contracted gallbladder typically involves imaging tests. Ultrasound is the most common and non-invasive method used to visualize the gallbladder. It can detect gallstones, inflammation, and the size and shape of the gallbladder.
Other diagnostic tools may include a hepatobiliary iminodiacetic acid (HIDA) scan, which assesses the functioning of the gallbladder and bile ducts, and MRI or CT scans for more detailed images.
Treatment Options

Treatment for a contracted gallbladder depends on the underlying cause.
In cases where gallstones or inflammation are the causes, treatment may involve medication to dissolve gallstones or surgery to remove the gallbladder (cholecystectomy).
In less severe cases or where surgery is not an option, dietary modifications and medications to manage symptoms might be recommended.
Biliary dyskinesia, a functional gallbladder disorder, is often treated with medications that improve bile flow and dietary changes.
Lifestyle and Diet Modifications

Beyond medical therapies, adopting certain lifestyle and dietary changes is crucial for managing symptoms related to a contracted or dysfunctional gallbladder. Clinical guidelines consistently emphasize that what you eat—and how you eat—can significantly impact both the frequency and severity of symptoms.
A diet low in fat and high in fiber is considered one of the most effective strategies. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), reducing dietary fat lessens the workload on the gallbladder, as fatty foods trigger its contraction and can provoke pain or discomfort in susceptible individuals. Fiber, found in fruits, vegetables, and whole grains, helps regulate digestion and may support bile flow.
Recommended dietary strategies include:
-
Eat smaller, more frequent meals: Large, heavy meals can overtax the digestive system. By eating 4–6 smaller meals per day, you reduce the chances of sudden, forceful gallbladder contractions.
-
Avoid high-fat and fried foods: Foods like bacon, butter, cream sauces, fried snacks, and processed meats should be minimized or eliminated. The Cleveland Clinic recommends keeping total daily fat intake to less than 30% of total calories for those with gallbladder problems.
-
Increase fruits, vegetables, and whole grains: These foods are high in fiber, vitamins, and antioxidants. Examples include apples, leafy greens, oats, brown rice, lentils, and carrots.
-
Limit refined sugars and processed foods: Sweets, sugary drinks, and processed snacks can worsen digestive symptoms and contribute to weight gain.
Lifestyle modifications:
-
Regular physical activity: Engaging in moderate exercise—such as brisk walking, cycling, or swimming—improves digestion and supports healthy weight. Research published in the American Journal of Gastroenterology suggests that regular exercise lowers the risk of developing symptomatic gallstones and gallbladder attacks.
-
Maintain a healthy weight: Obesity increases the risk of gallbladder disease, but rapid weight loss can also trigger gallstone formation. Aim for gradual, sustainable weight reduction if needed.
-
Hydration: Drinking enough water supports digestion and overall health.
Table: Gallbladder-Friendly Eating Habits
| Do | Avoid |
|---|---|
| Eat small, frequent meals | Large, fatty, or fried meals |
| Choose lean proteins | Processed or red meats |
| Add fiber-rich fruits/veggies | Sugary snacks, soft drinks |
| Opt for whole grains | White bread, pastries |
| Stay hydrated | Alcohol, high-fat dairy |
Monitoring and Follow-up
Regular monitoring and follow-up are crucial for individuals diagnosed with a contracted gallbladder, especially when it is linked to gallbladder disease or other underlying conditions. Follow-up appointments with a healthcare provider typically include physical examinations, discussions about symptoms, and possibly repeated imaging tests.
These follow-up sessions help in assessing the effectiveness of the treatment and making necessary adjustments. They also serve to monitor for potential complications such as gallbladder rupture or the development of gallstones.
Non-Surgical Therapies
For individuals who are unable or unwilling to undergo surgery—such as cholecystectomy (gallbladder removal)—a variety of non-surgical options may be considered for managing gallbladder disease or a contracted gallbladder. According to the American College of Gastroenterology, these therapies are especially relevant for older adults, those with significant comorbidities, or patients who prefer to avoid surgery.
Non-surgical management may include:
-
Medications:
Pain relievers (such as acetaminophen or prescription analgesics) and anti-inflammatory drugs can help control symptoms. In some cases, antispasmodic medications are used to reduce biliary colic. -
Gallstone-dissolving treatments:
Oral bile acid pills, such as ursodeoxycholic acid, may gradually dissolve cholesterol gallstones. However, this method is generally reserved for patients who cannot have surgery, as it can take months or years and is only effective for certain types of stones (Mayo Clinic). -
Lifestyle interventions:
Dietary modifications (as detailed in the previous section) are often a first-line approach to minimize symptoms and reduce flare-ups. Weight management, regular exercise, and careful monitoring of fat intake are especially important. -
Endoscopic or radiologic interventions:
In some cases, minimally invasive procedures such as ERCP (endoscopic retrograde cholangiopancreatography) may be used to remove bile duct stones or relieve obstructions.
Complications and Risks
Understanding the potential complications and risks associated with a contracted gallbladder, whether treated surgically or non-surgically, is important. Complications can include infection, bile duct injury, and in rare cases, gallbladder cancer.
Chronic gallbladder disease without proper treatment can lead to serious issues such as a ruptured gallbladder. Being aware of these risks allows for timely intervention and prevention.
Preventive Measures

Prevention plays a pivotal role in reducing the risk of gallbladder problems and their complications. Key preventive strategies include:
- Obesity is a major risk factor for gallstones and gallbladder disease. However, avoid rapid weight loss, which can also trigger gallstone formation, as noted by the Cleveland Clinic.
- Emphasize a diet low in saturated fats and high in fiber—plenty of fruits, vegetables, and whole grains. Limit processed foods and excessive sugars.
- Routine exercise helps regulate cholesterol levels and supports healthy digestion.
- Keep conditions like high cholesterol, diabetes, and metabolic syndrome well-controlled, as these can increase gallbladder risk.
- Regular medical evaluations and screening can lead to early detection of gallbladder or liver issues, improving the chances of effective management and prevention of complications.
| Preventive Measure | How It Helps |
|---|---|
| Maintain healthy weight | Reduces gallstone risk |
| Balanced, low-fat, high-fiber diet | Minimizes gallbladder stress |
| Regular exercise | Improves metabolism & cholesterol |
| Control diabetes/cholesterol | Lowers risk of gallstones |
| Routine check-ups | Enables early detection/treatment |
FAQs
Can a contracted gallbladder lead to digestive problems?
Yes, a contracted gallbladder can lead to digestive issues. Since the gallbladder plays a role in storing and releasing bile for fat digestion, its abnormal contraction can affect this process, leading to symptoms like indigestion, bloating, and changes in bowel movements.
How quickly do symptoms appear if a contracted gallbladder is due to gallstones?
Symptoms due to gallstones in a contracted gallbladder can vary. Some people might experience sudden and intense pain, while others may have gradual onset of symptoms. The timing of symptom appearance can also depend on factors like the size and location of the gallstones.
Are there any specific tests to confirm that a gallbladder is contracted due to gallstones?
Ultrasound is the primary tool for detecting gallstones in a contracted gallbladder. However, if the ultrasound is inconclusive, a HIDA scan or an MRI may be performed to provide more detailed images and confirm the presence of gallstones.
Can lifestyle changes alone resolve a contracted gallbladder?
Lifestyle changes, such as a healthier diet and regular exercise, can alleviate some symptoms associated with a contracted gallbladder, especially if related to diet or obesity. However, they may not resolve all causes, such as gallstones or chronic inflammation, which might require medical or surgical intervention.
Is a contracted gallbladder a common condition in pregnant women?
Pregnant women may experience gallbladder contraction more frequently, as hormonal changes can slow gallbladder movement and lead to gallstone formation. Also, the growing uterus can physically affect the gallbladder’s position, impacting its function.
After gallbladder removal, can the gallbladder contract again or cause symptoms?
Once the gallbladder is removed (cholecystectomy), it cannot contract or cause direct symptoms. However, some individuals may experience changes in digestion or develop a condition called postcholecystectomy syndrome, which can mimic gallbladder-related symptoms.
Final Words
A contracted gallbladder can range from a normal physiological response to a sign of an underlying health issue. Diagnosis involves imaging tests and possibly further examinations to determine the cause. Treatment varies from dietary changes and medications to surgical interventions, depending on the severity and underlying cause.
Regular monitoring, understanding the risks and complications, and taking preventive measures are key to managing this condition effectively. Working closely with healthcare providers to develop a personalized treatment plan is essential for optimal health and quality of life.
Related Posts:
- Gallbladder Calculus and Acute Cholecystitis -…
- What is Incarcerated Hernias? - Causes, Symptoms,…
- Flat Feet in Children - Diagnosis and Treatment…
- Effective Treatment Options for Arthritis and Joint Pain
- Lumbar Spine Pain - Causes, Symptoms, And Treatment Options
- How to Treat a Blood Clot in Your Leg - DVT…















